Arch Pain Treatment
Overview
Your foot has an incredible design. All of the parts fit together in such a way as to be flexible and moveable while still being very strong. One of the important parts of the foot is your arch. Located in the middle of your foot, it is slightly raised off the ground and helps you absorb the impact of every step. Sometimes, however, it can ache and make walking or standing around very uncomfortable.

Causes
The arch of the foot is the concaved, mid-section of the sole. While it only spans an inch or two in most adults, this one small area of the foot bears nearly all of your weight when you walk, and helps to transfer this weight from heel to ball. Just beneath the skin on the sole of the foot, a tough, elastic ligament called the plantar fascia extends from your heel bone to the metatarsal area of the foot. This ligament is designed to bounce gently with the spring of your step, but a number of factors can cause it to become unhealthy. These include. An abnormal walking gait. Vigorous high-impact exercise such as running, playing tennis or basketball. Being overweight. Wearing shoes that slant or cramp any part of the foot. Wearing shoes that have worn down in the heel or sole. A traumatic injury to the foot, including cuts, bruises, strains and fractures. The presence of arthritis or other inflammatory conditions. The normal aging process. In the presence of any of the above factors, the plantar fascia ligament can begin to flex beyond its normal range of motion. Small tears may develop in the tissue and inflammation is commonly present. You may describe your arch pain as sore, sharp, tender, intermittent, constant, burning, tingling or aching. All of these adjectives may be signs that you are experiencing a condition called Plantar Fasciitis.
Symptoms
Symptoms of plantar fasciitis may occur anywhere along the arch, but it is most common near its attachment to the heel bone. Symptoms of plantar fasciitis vary, but the classic symptom is pain after rest--when you first get out of bed in the morning, or when you get up after sitting down for a while during the day. This is known as "post-static dyskinesia." The pain usually diminishes after a few minutes of walking, sometimes even disappearing, but the pain is commonly felt again the longer you're on the foot. Fasciitis can be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation of long-periods of standing, especially on concrete, and by being overweight. Other factors which influence this condition are gender (females get this more than men), age (30s to 50s are most common), and those with flatter-than-normal feet. It doesn't help that fascia doesn't heal particularly quickly. This is because it has relatively poor circulation, which is why it's white in colour.
Diagnosis
Diagnosis of a plantar plate tear can often be challenging due to the complex nature of the anatomy of the foot. Careful history taking and an examination of the area of pain is required to determine the extent and cause of the tear. If necessary, further investigations such as x-rays or diagnostic ultrasound may be ordered by your podiatrist to help evaluate the severity of the problem.
Non Surgical Treatment
An orthotic arch support, specially molded to fit your foot, may be part of your treatment. These supports can be particularly helpful if you have flat feet or high arches. You can tell if that is what is needed when short-term taping decreases your heel pain.

Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions.
Prevention
There are several things that you can do to prevent and treat arch pain. This includes Avoiding high heeled shoes, Stretching the calf muscles regularly, Wearing well fitted, comfortable shoes, Using customisedorthotic devices or shoe inserts, Elevating the feet and applying ice and taking over-the-counter anti-inflammatory medications. You can also care for your feet by paying attention to any changes in your feet as you get older. It is normal for feet to lose some of their fat pads as a person ages. Your feet may get bigger, both wider and longer as well. Make sure that you wear shoes that are sturdy, but comfortable, and have your feet measured before you buy shoes to make sure that you are still wearing the right size. Shoe sizes vary from one brand to the next, so it is a good idea to have your feet measured every time you purchase shoes. When choosing shoes, match the shoe to the activity for which it will be worn. Within the broader grouping of athletic shoes, there are different categories with different features. For example, a running shoe has different features than a walking shoe. You may develop some arthritic changes in your feet over time, too. If you notice that you are experiencing more pain in your feet, see your doctor for an evaluation. If the pain is arthritis-related, your doctor may recommend medication or other treatment to slow the progression of the arthritis.
Your foot has an incredible design. All of the parts fit together in such a way as to be flexible and moveable while still being very strong. One of the important parts of the foot is your arch. Located in the middle of your foot, it is slightly raised off the ground and helps you absorb the impact of every step. Sometimes, however, it can ache and make walking or standing around very uncomfortable.

Causes
The arch of the foot is the concaved, mid-section of the sole. While it only spans an inch or two in most adults, this one small area of the foot bears nearly all of your weight when you walk, and helps to transfer this weight from heel to ball. Just beneath the skin on the sole of the foot, a tough, elastic ligament called the plantar fascia extends from your heel bone to the metatarsal area of the foot. This ligament is designed to bounce gently with the spring of your step, but a number of factors can cause it to become unhealthy. These include. An abnormal walking gait. Vigorous high-impact exercise such as running, playing tennis or basketball. Being overweight. Wearing shoes that slant or cramp any part of the foot. Wearing shoes that have worn down in the heel or sole. A traumatic injury to the foot, including cuts, bruises, strains and fractures. The presence of arthritis or other inflammatory conditions. The normal aging process. In the presence of any of the above factors, the plantar fascia ligament can begin to flex beyond its normal range of motion. Small tears may develop in the tissue and inflammation is commonly present. You may describe your arch pain as sore, sharp, tender, intermittent, constant, burning, tingling or aching. All of these adjectives may be signs that you are experiencing a condition called Plantar Fasciitis.
Symptoms
Symptoms of plantar fasciitis may occur anywhere along the arch, but it is most common near its attachment to the heel bone. Symptoms of plantar fasciitis vary, but the classic symptom is pain after rest--when you first get out of bed in the morning, or when you get up after sitting down for a while during the day. This is known as "post-static dyskinesia." The pain usually diminishes after a few minutes of walking, sometimes even disappearing, but the pain is commonly felt again the longer you're on the foot. Fasciitis can be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation of long-periods of standing, especially on concrete, and by being overweight. Other factors which influence this condition are gender (females get this more than men), age (30s to 50s are most common), and those with flatter-than-normal feet. It doesn't help that fascia doesn't heal particularly quickly. This is because it has relatively poor circulation, which is why it's white in colour.
Diagnosis
Diagnosis of a plantar plate tear can often be challenging due to the complex nature of the anatomy of the foot. Careful history taking and an examination of the area of pain is required to determine the extent and cause of the tear. If necessary, further investigations such as x-rays or diagnostic ultrasound may be ordered by your podiatrist to help evaluate the severity of the problem.
Non Surgical Treatment
An orthotic arch support, specially molded to fit your foot, may be part of your treatment. These supports can be particularly helpful if you have flat feet or high arches. You can tell if that is what is needed when short-term taping decreases your heel pain.

Surgical Treatment
In cases where cast immobilization, orthoses and shoe therapy have failed, surgery is the next alternative. The goal of surgery and non-surgical treatment is to eliminate pain, stop progression of the deformity and improve mobility of the patient. Opinions vary as to the best surgical treatment for adult acquired flatfoot. Procedures commonly used to correct the condition include tendon debridement, tendon transfers, osteotomies (cutting and repositioning of bone) and joint fusions.
Prevention
There are several things that you can do to prevent and treat arch pain. This includes Avoiding high heeled shoes, Stretching the calf muscles regularly, Wearing well fitted, comfortable shoes, Using customisedorthotic devices or shoe inserts, Elevating the feet and applying ice and taking over-the-counter anti-inflammatory medications. You can also care for your feet by paying attention to any changes in your feet as you get older. It is normal for feet to lose some of their fat pads as a person ages. Your feet may get bigger, both wider and longer as well. Make sure that you wear shoes that are sturdy, but comfortable, and have your feet measured before you buy shoes to make sure that you are still wearing the right size. Shoe sizes vary from one brand to the next, so it is a good idea to have your feet measured every time you purchase shoes. When choosing shoes, match the shoe to the activity for which it will be worn. Within the broader grouping of athletic shoes, there are different categories with different features. For example, a running shoe has different features than a walking shoe. You may develop some arthritic changes in your feet over time, too. If you notice that you are experiencing more pain in your feet, see your doctor for an evaluation. If the pain is arthritis-related, your doctor may recommend medication or other treatment to slow the progression of the arthritis.
Achilles Tendon Sore To The Touch
Overview
 Achilles tendinitis is an irritation/inflammation in the achilles tendon, which attaches to the back of the heel. It is often a result of overuse and occurs frequently in runners who have altered their training suddenly, either with regard to duration or intensity. This injury is also prevalent in middle-aged people who are active.
Achilles tendinitis is an irritation/inflammation in the achilles tendon, which attaches to the back of the heel. It is often a result of overuse and occurs frequently in runners who have altered their training suddenly, either with regard to duration or intensity. This injury is also prevalent in middle-aged people who are active.
Causes
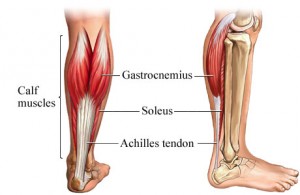
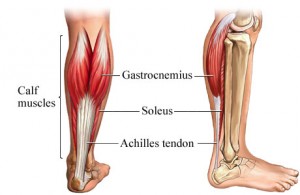
There are two large muscles in the calf. These muscles are important for walking. They create the power needed to push off with the foot or go up on the toes. The large Achilles tendon connects these muscles to the heel. Heel pain is most often due to overuse of the foot. Rarely it is caused by an injury. Tendinitis due to overuse is most common in younger people. It can occur in walkers, runners, or other athletes. Achilles tendinitis may be more likely to occur if you Suddenly increase the amount or intensity of an activity. Your calf muscles are very tight (not stretched out). You run on hard surfaces such as concrete. You run too often, you jump a lot (such as when playing basketball), you do not have shoes with proper support, your foot suddenly turns in or out. Tendinitis from arthritis is more common in middle-aged and elderly people. A bone spur or growth may form in the back of the heel bone. This may irritate the Achilles tendon and cause pain and swelling.
Symptoms
If you have Achilles tendinitis or Achilles enthesopathy, you are likely to experience the following symptoms. Pain. You may notice aching, burning, or tearing pains at the back of your heel or above the ankle. The pain can range from mild to very severe and disabling. It is most noticeable in the following circumstances. After resting. Many people report that pain increases when they first get out of bed in the morning or after sitting for a period of time. After exercise. Pain may increase if you exercise or stand for a period of time. A lump. In some cases, a tender lump can develop at the site of the injured tendon (tendinosis). Bone spurs. When the injury occurs at the point where the tendon attaches to the foot, a bone spur may develop on the heel.
Diagnosis
A doctor or professional therapist will confirm a diagnosis, identify and correct possible causes, apply treatment and prescribe eccentric rehabilitation exercises. An MRI or Ultrasound scan can determine the extent of the injury and indicate a precise diagnosis. Gait analysis along with a physical assessment will identify any possible biomechanical factors such as over pronation which may have contributed to the achilles tendonitis and training methods will be considered. Biomechanical problems can be corrected with the use of orthotic inserts and selection of correct footwear.
Nonsurgical Treatment
The aim of the treatment is to reduce strain on the tendon and reduce inflammation. Strain may be reduced by, avoiding or severely limiting activities that may aggravate the condition, such as running, using shoe inserts (orthoses) to take pressure off the tendon as it heals. In cases of flat or hyperpronated feet, your doctor or podiatrist may recommend long-term use of orthoses. I8nflammation may be reduced by, applying icepacks for 20 minutes per hour during the acute stage, taking non-steroidal anti-inflammatory drugs, placing the foot in a cast or restrictive ankle-boot to minimise movement and give the tendon time to heal. This may be recommended in severe cases and used for about eight weeks. Occasionally depot (slowly absorbed) steroid injections may be tried, particularly for peri-tendinitis, but great care needs to be taken to avoid injecting into the tendon. This should only be done by a specialist doctor. You may also be given specific exercises to gently stretch the calf muscles once the acute stage of inflammation has settled down. Your doctor or physiotherapist will recommend these exercises when you are on the road to recovery. Recovery is often slow and will depend on the severity of the condition and how carefully you follow the treatment and care instructions you are given.
Surgical Treatment
Not every Achilles tendon injury or condition requires surgery. It is generally understood by doctors and surgeons, that surgery will introduce more scar tissue into the Achilles tendon. This added scar tissue will be problematic, requiring physical therapy and conservative treatment options post-surgery. If not dealt with properly, your ankle and Achilles tendon could end up in worse condition than before the surgery! This is why surgery is only performed as a last resort.
Prevention
To prevent Achilles tendonitis or tendonosis from recurring after surgical or non-surgical treatment, the foot and ankle surgeon may recommend strengthening and stretching of the calf muscles through daily exercises. Wearing proper shoes for the foot type and activity is also important in preventing recurrence of the condition.
 Achilles tendinitis is an irritation/inflammation in the achilles tendon, which attaches to the back of the heel. It is often a result of overuse and occurs frequently in runners who have altered their training suddenly, either with regard to duration or intensity. This injury is also prevalent in middle-aged people who are active.
Achilles tendinitis is an irritation/inflammation in the achilles tendon, which attaches to the back of the heel. It is often a result of overuse and occurs frequently in runners who have altered their training suddenly, either with regard to duration or intensity. This injury is also prevalent in middle-aged people who are active.
Causes
There are two large muscles in the calf. These muscles are important for walking. They create the power needed to push off with the foot or go up on the toes. The large Achilles tendon connects these muscles to the heel. Heel pain is most often due to overuse of the foot. Rarely it is caused by an injury. Tendinitis due to overuse is most common in younger people. It can occur in walkers, runners, or other athletes. Achilles tendinitis may be more likely to occur if you Suddenly increase the amount or intensity of an activity. Your calf muscles are very tight (not stretched out). You run on hard surfaces such as concrete. You run too often, you jump a lot (such as when playing basketball), you do not have shoes with proper support, your foot suddenly turns in or out. Tendinitis from arthritis is more common in middle-aged and elderly people. A bone spur or growth may form in the back of the heel bone. This may irritate the Achilles tendon and cause pain and swelling.
Symptoms
If you have Achilles tendinitis or Achilles enthesopathy, you are likely to experience the following symptoms. Pain. You may notice aching, burning, or tearing pains at the back of your heel or above the ankle. The pain can range from mild to very severe and disabling. It is most noticeable in the following circumstances. After resting. Many people report that pain increases when they first get out of bed in the morning or after sitting for a period of time. After exercise. Pain may increase if you exercise or stand for a period of time. A lump. In some cases, a tender lump can develop at the site of the injured tendon (tendinosis). Bone spurs. When the injury occurs at the point where the tendon attaches to the foot, a bone spur may develop on the heel.
Diagnosis
A doctor or professional therapist will confirm a diagnosis, identify and correct possible causes, apply treatment and prescribe eccentric rehabilitation exercises. An MRI or Ultrasound scan can determine the extent of the injury and indicate a precise diagnosis. Gait analysis along with a physical assessment will identify any possible biomechanical factors such as over pronation which may have contributed to the achilles tendonitis and training methods will be considered. Biomechanical problems can be corrected with the use of orthotic inserts and selection of correct footwear.
Nonsurgical Treatment
The aim of the treatment is to reduce strain on the tendon and reduce inflammation. Strain may be reduced by, avoiding or severely limiting activities that may aggravate the condition, such as running, using shoe inserts (orthoses) to take pressure off the tendon as it heals. In cases of flat or hyperpronated feet, your doctor or podiatrist may recommend long-term use of orthoses. I8nflammation may be reduced by, applying icepacks for 20 minutes per hour during the acute stage, taking non-steroidal anti-inflammatory drugs, placing the foot in a cast or restrictive ankle-boot to minimise movement and give the tendon time to heal. This may be recommended in severe cases and used for about eight weeks. Occasionally depot (slowly absorbed) steroid injections may be tried, particularly for peri-tendinitis, but great care needs to be taken to avoid injecting into the tendon. This should only be done by a specialist doctor. You may also be given specific exercises to gently stretch the calf muscles once the acute stage of inflammation has settled down. Your doctor or physiotherapist will recommend these exercises when you are on the road to recovery. Recovery is often slow and will depend on the severity of the condition and how carefully you follow the treatment and care instructions you are given.
Surgical Treatment
Not every Achilles tendon injury or condition requires surgery. It is generally understood by doctors and surgeons, that surgery will introduce more scar tissue into the Achilles tendon. This added scar tissue will be problematic, requiring physical therapy and conservative treatment options post-surgery. If not dealt with properly, your ankle and Achilles tendon could end up in worse condition than before the surgery! This is why surgery is only performed as a last resort.
Prevention
To prevent Achilles tendonitis or tendonosis from recurring after surgical or non-surgical treatment, the foot and ankle surgeon may recommend strengthening and stretching of the calf muscles through daily exercises. Wearing proper shoes for the foot type and activity is also important in preventing recurrence of the condition.
What Is Pes Planus?
Overview

Most of us have a low arch. The foot actually appears quite normal and a clear (but low) arch is present under the foot, especially when sitting down. The situation changes with weight bearing: when we get up the arch lowers. When we start walking the arches collapse and the ankles roll inwards. This is called over-pronation - or fallen arches. Over-pronation is not the same as flat feet as often noted. Pronation itself is not wrong as we need to pronate and supinate as part of our gait. Pronation (rolling in) acts as a shock absorbing process and supination (rolling out) helps to propel our feet forward.
Causes
Turning 40 doesn?t necessarily have anything to do with it, but over time you?ve likely engaged in certain activities or developed some unhealthy habits that led to this condition. If you are overweight, you are placing excess burdens on your feet, causing the tendons to strain. Some women experience fallen arches because of weight gain during pregnancy. You also may have damaged these tendons while exercising. If you suffered a serious injury to the foot, you may have weakened the tendons, which can also lead to this development.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
Many medical professionals can diagnose a flat foot by examining the patient standing or just looking at them. On going up onto tip toe the deformity will correct when this is a flexible flat foot in a child with lax joints. Such correction is not seen in the adult with a rigid flat foot. An easy and traditional home diagnosis is the "wet footprint" test, performed by wetting the feet in water and then standing on a smooth, level surface such as smooth concrete or thin cardboard or heavy paper. Usually, the more the sole of the foot that makes contact (leaves a footprint), the flatter the foot. In more extreme cases, known as a kinked flatfoot, the entire inner edge of the footprint may actually bulge outward, where in a normal to high arch this part of the sole of the foot does not make contact with the ground at all.
Non Surgical Treatment
Heel cord stretching is an important part of treatment, as a tight Achilles tendon tends to pronate the foot. Orthotics (inserts or insoles, often custom-made) may be used. These usually contain a heel wedge to correct calcaneovalgus deformity, and an arch support. This is the usual treatment for flexible Pes Planus (if treatment is needed). A suitable insole can help to correct the deformity while it is worn. Possibly it may prevent progression of flat feet, or may reduce symptoms. However, the effectiveness of arch support insoles is uncertain. Arch supports used without correcting heel cord contracture can make symptoms worse. In patients with fixed Pes planus or arthropathy, customised insoles may relieve symptoms. Reduce contributing factors, wear shoes with low heels and wide toes. Lose weight if appropriate. Do exercises to strengthen foot muscles - walking barefoot (if appropriate), toe curls (flexing toes) and heel raises (standing on tiptoe).
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.

Most of us have a low arch. The foot actually appears quite normal and a clear (but low) arch is present under the foot, especially when sitting down. The situation changes with weight bearing: when we get up the arch lowers. When we start walking the arches collapse and the ankles roll inwards. This is called over-pronation - or fallen arches. Over-pronation is not the same as flat feet as often noted. Pronation itself is not wrong as we need to pronate and supinate as part of our gait. Pronation (rolling in) acts as a shock absorbing process and supination (rolling out) helps to propel our feet forward.
Causes
Turning 40 doesn?t necessarily have anything to do with it, but over time you?ve likely engaged in certain activities or developed some unhealthy habits that led to this condition. If you are overweight, you are placing excess burdens on your feet, causing the tendons to strain. Some women experience fallen arches because of weight gain during pregnancy. You also may have damaged these tendons while exercising. If you suffered a serious injury to the foot, you may have weakened the tendons, which can also lead to this development.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
Many medical professionals can diagnose a flat foot by examining the patient standing or just looking at them. On going up onto tip toe the deformity will correct when this is a flexible flat foot in a child with lax joints. Such correction is not seen in the adult with a rigid flat foot. An easy and traditional home diagnosis is the "wet footprint" test, performed by wetting the feet in water and then standing on a smooth, level surface such as smooth concrete or thin cardboard or heavy paper. Usually, the more the sole of the foot that makes contact (leaves a footprint), the flatter the foot. In more extreme cases, known as a kinked flatfoot, the entire inner edge of the footprint may actually bulge outward, where in a normal to high arch this part of the sole of the foot does not make contact with the ground at all.
Non Surgical Treatment
Heel cord stretching is an important part of treatment, as a tight Achilles tendon tends to pronate the foot. Orthotics (inserts or insoles, often custom-made) may be used. These usually contain a heel wedge to correct calcaneovalgus deformity, and an arch support. This is the usual treatment for flexible Pes Planus (if treatment is needed). A suitable insole can help to correct the deformity while it is worn. Possibly it may prevent progression of flat feet, or may reduce symptoms. However, the effectiveness of arch support insoles is uncertain. Arch supports used without correcting heel cord contracture can make symptoms worse. In patients with fixed Pes planus or arthropathy, customised insoles may relieve symptoms. Reduce contributing factors, wear shoes with low heels and wide toes. Lose weight if appropriate. Do exercises to strengthen foot muscles - walking barefoot (if appropriate), toe curls (flexing toes) and heel raises (standing on tiptoe).
Surgical Treatment

Feet that do not respond to the treatments above may need surgery. The surgery will help to create a supportive arch.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.